Spoiler: It’s not about fixing them. It’s about listening.
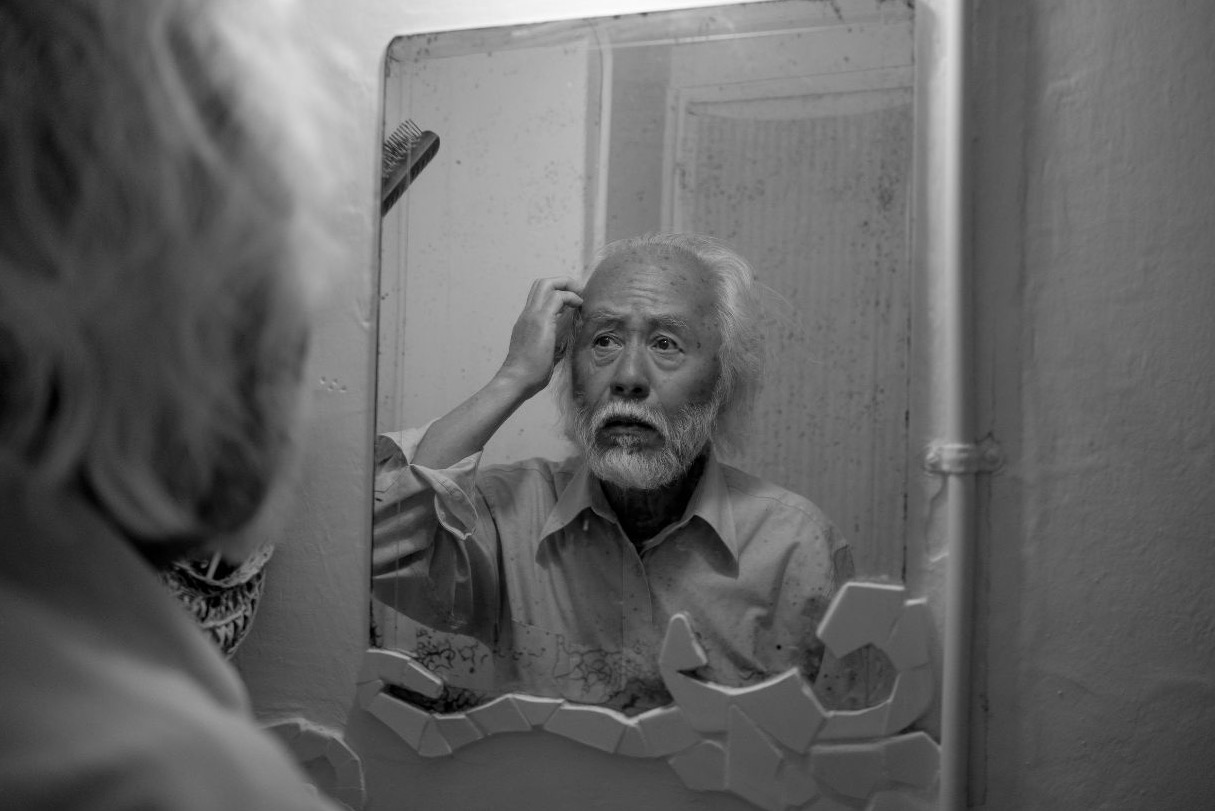
Let’s start with a big truth: mental health matters at every age. Whether you’re 27 or 87, how we feel emotionally, psychologically, and socially affects how we show up in the world. And for older adults—who may be navigating some big life changes like the loss of a partner, a new medical diagnosis, or shifts in independence—mental health becomes especially important.
But talking about it? That can get complicated. There’s a lot of stigma. A lot of outdated myths. A lot of “we didn’t talk about that in my day” energy.
So, let’s walk through how to open up conversations about mental health with the older adults in your life—with respect, compassion, and a clear sense of what’s actually helpful.

🚨 First: Know the Signs Something Might Be Off
Mental health challenges can look different in older adults. Here are some things to watch for:
- Mood changes or increased irritability
- Loss of interest in activities they once enjoyed
- Sleep disturbances (too much or too little)
- Digestive issues or frequent headaches
- Difficulty concentrating
- Emotional numbness or persistent sadness
- Anxiety, worry, or obsessive thinking
- Substance misuse
- Talking about feeling hopeless or like a burden
- Engaging in risky behaviors
And remember: mental health symptoms are not just part of “getting old.” Depression, anxiety, and other conditions deserve to be taken seriously—and treated.
🌪 What Causes Mental Health Struggles Later in Life?
Plenty of things can shake our emotional footing. For older adults, that list might include:
- Grief and loss
- Isolation or loneliness
- Chronic pain or illness
- Retirement and identity changes
- Cognitive decline or dementia
- Big life transitions
Sometimes, it’s not even clear what the cause is—just that things feel off. And that’s enough reason to start a conversation.
🧠 Mental Health Conditions You Might Be Seeing
It’s not about labeling, but a general understanding helps. Here are some common conditions:
- Depression (including seasonal, major, or bipolar)
- Anxiety disorders (like GAD, panic disorder, or specific phobias)
- Obsessive-compulsive disorder (OCD)
- Borderline personality disorder (BPD)
- Eating disorders (yes, they can show up at any age)
- Sundowning (late-day confusion common in dementia)

*It is important to remember that quirks or preferences (like needing to have your clothes in rainbow order) do not mean you have a mental illness or disorder. The World Health Organization defines mental disorder as
“A mental disorder is characterized by a clinically significant disturbance in an individual’s cognition, emotional regulation, or behaviour. It is usually associated with distress or impairment in important areas of functioning. “

🗣 How to Start the Conversation
You don’t need a therapy degree to be supportive. You just need compassion and a bit of strategy.
Try something like:
“You’ve been through a lot lately. I wonder if it’s been affecting how you’re feeling emotionally. Would you be open to talking about what support might look like?”
If they say yes, you can gently offer:
“Sometimes these changes are connected to what’s happening in the body—and sometimes it’s emotional stuff, too. Either way, there’s help available. Maybe we can talk to your doctor about it and see what they recommend?”
Normalize, validate, and be curious, not pushy.
🧍♀️What If They Say No?
That’s okay. Truly.
Older adults—just like anyone—have the right to make decisions about their care. If they’re not ready, try:
“I hear that. It might not feel like the right time. Just know, if you change your mind, I’m here to help you.”
And then leave the door open. No pressure. No guilt-tripping. That’s how trust builds.
❌ Busting Common Mental Health Myths in Older Adults
Let’s clear a few things up:
- Myth: Depression is just part of aging.
❌ Nope. It’s common, but not normal—and it deserves treatment.
- Myth: Older people can’t change.
❌ Not true. Older adults benefit from therapy, medication, and support just as much as anyone.
- Myth: Talking about it makes it worse.
❌ The opposite. Silence adds shame. Talking opens the door to healing.


❤️ If You’re the One Struggling
Maybe you’re not just here for someone else—maybe you are an older adult who’s feeling off, overwhelmed, or like you’re not yourself.
Here’s the thing: there’s nothing shameful about that. Mental health conditions are common, treatable, and not your fault.
Talk to someone you trust. Call your doctor. Reach out to a mental health professional. Or just start with one small conversation.
You are not alone. And you don’t have to carry this by yourself.
📞 If You or Someone You Know is in Crisis
Call or text the Suicide & Crisis Lifeline at 988.
If it’s an emergency, dial 911 or go to your nearest emergency room.
Your life matters. You are not alone.
Final Thoughts
Supporting the mental health of older adults isn’t about swooping in to “fix” something. It’s about listening. Validating. Gently guiding when it’s welcome—and backing off when it’s not.
Your job isn’t to convince someone to get help. Your job is to show up with care, let them know what help is available, and respect their right to decide.
Because mental health is health—and older adults deserve support that honors their experiences, dignity, and choices.
Recent Comments