Understanding Dementia Behaviors: Seeing the Person, Not the Diagnosis
et’s dive into something I see a lot when working with folks living with dementia: uncharacteristic behaviors.
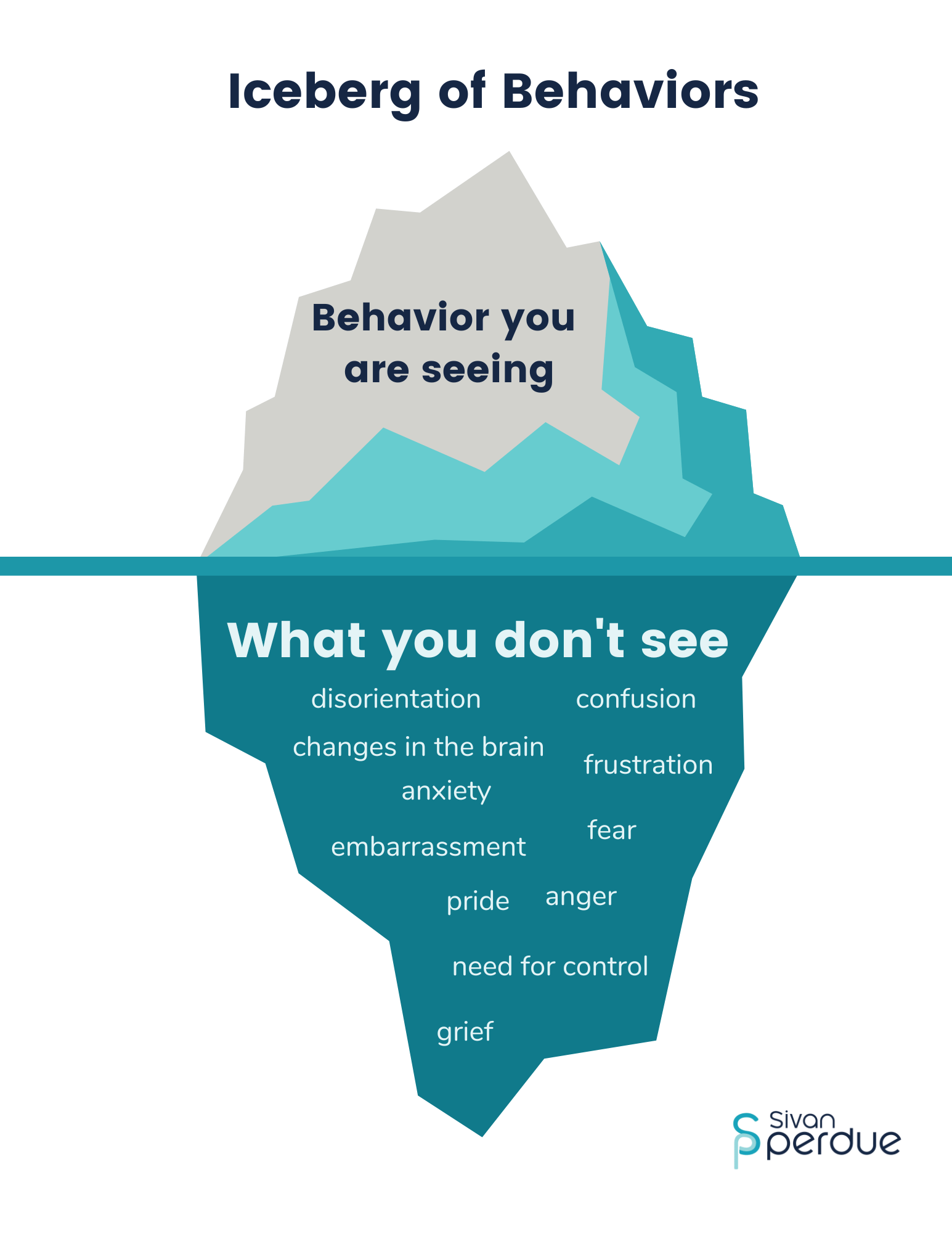
These behaviors — whether confusing, frustrating, or sometimes even funny — are often a form of communication. Once you recognize that, it becomes a game changer in how you interact with your loved one. Instead of seeing these behaviors as stubbornness or defiance, you can start asking, “What are they trying to tell me?”
Let’s break down a few common behaviors and how to approach them with empathy, connection, curiosity, and a focus on the person, not just the diagnosis.
1. Anger and Frustration: It’s Not Just a Bad Mood
Anger often comes from feeling:
- Scared: The world doesn’t make sense, and that’s terrifying.
- Embarrassed: They know something’s off — they’re aware enough to realize they should remember or recognize something, but can’t.
- Humiliated: Struggling with things they used to do easily (like putting on a sweater or brushing their teeth) is incredibly frustrating.
None of us like to be wrong, right? Imagine being constantly corrected when your brain is already doing its best to hold on. That can lead to pushback — even anger. Even when you are not living with dementia, when anger shows up, it is usually about another feel that we do not know how to express.
Caregiving tip: Instead of correcting them, meet them where they are. Validate their feelings. You might say, “That sounds frustrating,” or gently change the subject if it’s not essential to correct the details.
2. Depression: More Than Just a Symptom
Depression is common, especially in the early stages of dementia. And here’s the thing — it often gets overlooked because the symptoms (like memory loss and isolation) overlap with dementia itself.
A big part of this comes from loss:
- Loss of identity
- Loss of control
- Loss of autonomy
People tend to focus on the diagnosis and treatment, and the person can get lost in the shuffle. That social withdrawal? It’s often not just dementia — it’s grief and loss too.
What can help: Acknowledge and honor their emotions, find activities they still enjoy, and seek professional support when needed. Remember, Depression is very easily treated and when done so, can often reduce some of those challenging behaviors.

3. Anxiety: Clinginess and Fear Responses
Anxiety often shows up as:
- Isolation and not wanting to leave the house
- Pacing and restlessness
- Clinging to familiar people or objects
Why? Because as their memory of familiar places and people fades, the world becomes a scary, unfamiliar place. So they hold on tight to what feels safe and predictable.
How to support: Create a calm, structured environment and stick to routines as much as possible. Familiarity brings comfort.
4. Mood Swings: Not Just “Bad Days”
Mood swings can stem from all sorts of things:
- Emotional factors: Fear, confusion, or untreated mental health conditions
- Physical discomfort: Pain, hunger, or fatigue (they might not be able to tell you they’re uncomfortable, but it’ll show up in their behavior)
- Environmental factors: Overstimulation, noise, clutter
This is where being a bit of a detective comes in handy. Ask yourself:
- Are they too hot, cold, or tired?
- Is there too much noise?
- Did something unfamiliar throw them off?
Sometimes small changes, like reducing background noise or simplifying a routine, can make a huge difference.
.


It’s Not Personal
Here’s a hard truth: Dementia can say hurtful things. But that’s the disease talking, not your loved one (which can be really difficult to remember when they are throwing very personal attacks at you). It’s crucial to get a bit of distance from those outbursts and remember that they would likely react the same way with anyone in that caregiving role.
Behavior = Communication
At the core of it all, behaviors are communication. They’re saying, “I’m scared,” “I’m confused,” or “Something doesn’t feel right.” When we shift our perspective and respond with compassion, we can create a more supportive and loving environment for our loved ones.
If you’re navigating this tricky terrain, know that you’re not alone. Caregiving is tough, and it’s okay to need help or community support.
Until next time, keep focusing on the person and maintaining connection, not just the symptoms of the diagnosis.
Recent Comments